
Photos and images provided by the authors.
By Douglas Bohl, PhD, AEMT, and Christopher Towler, PT, DPT, GCS, CEEAA, AEMT-P
The COVID-19 pandemic has resulted in severe shortages in personal protective equipment (PPE). Supplies of PPE that were normally on hand in both prehospital and hospital settings were in danger of rapid depletion as rate of the usage increased due to the pandemic. Once the availability of PPE improved, the cost had greatly increased, in some cases by over 300%. This stark reality necessitated the development of strategies to extend the supply of N95’s through reuse in hospital and prehospital settings. The COVID-19 pandemic has also reminded providers of the importance of PPE and effective equipment decontamination practices.
This article discusses the development of two ultraviolet (UV) decontamination systems that are inexpensive (~$350 in parts) and simple to construct by providers at a prehospital EMS agency. The first of these is a briefcase-sized unit that is designed to decontaminate N95 respirators allowing for reuse.
The second device is a UV “tower” that can be used to perform secondary decontamination in ambulances boxes and small rooms. In this article we detail the construction, light output performance of these units, and our protocols which were developed based on published scientific research. Our goal is to provide this information, including parts lists, to other prehospital or hospital agencies.
UV Decontamination Basics
Ultraviolet Germicidal Irradiation (UVGI) is a decontamination technique that uses UVC (254 nm) light to inactivate contaminant microorganisms. UV decontamination is currently used in a variety of settings including treatment of drinking water, indoor air, sterilization of medical devices, and secondary decontamination of medical facilities (e.g. patient rooms). There are several key aspects of this process that need to be understood for safe use.
First, the wavelength of the light is critical and bulbs must be specified as UVC or “germicidal” for this process to be effective. UVA and UVB bulbs will not perform the germicidal function and should not be used. Second, this is a light-based method therefore regions or objects in shadows will not receive UV light and will not be decontaminated.
And finally, this process is a disinfection, not a sterilization, process. The level of disinfection is discussed in terms of “log” reductions in live organisms. For example, a one-log reduction corresponds to a 90% reduction from the original concentration, two-log is 99%, 3-log is 99.9%, etc.
In order to develop protocols for UV decontamination, it is important to understand the basic terminology and behavior of light radiation. The power rating for bulbs (“watts”) is the power consumed during use of a bulb. The output power of a bulb is lower than the consumption, and for the UVC bulbs is slightly less than half of the consumed power. Irradiance, Ee, is the light radiation power over an area (mW/cm2). As light expands away from the bulb the irradiance decreases based on the distance squared.
For example, if the distance from the bulb is doubled the irradiance decreases by a factor of 4. The irradiance, Ee,x, at any location, x, can be found by measuring Ee,ref at a single reference location, xref, using the following equation:
![]()
The radiant exposure, He, is the amount of light energy received over an area (mJ/cm2). The radiant exposure at a specific location, He,x, is simply the irradiance at the surface location times the exposure time:
![]()
The radiant exposure can be thought of as the “dosage” required to neutralize the infectious contaminants. A useful analogy is drug administration, where the irradiance is analogous to the “concentration” of a medication and time would be analogous to the dose (time x irradiance) to be administered. The irradiance, and its variation with distance are important in the UV decontamination procedures because the user ultimately needs to know how long to illuminate a given area to neutralize desired pathogens.
The recent COVID-19 crisis has resulted in the use of UV decontamination on single use respirators.1-5 The most comprehensive source for information on decontamination of disposable respirators is found on the N95Decon website (n95decon.org). Interested readers are referred to this website as it summarizes the literature regarding the use of UV light (as well as other methods) for decontamination of single use respirators in a way that is easy to understand.
Decontamination of disposable respirators is complicated by several factors. First, respirators are a primary source of personal protection and decontamination failure poses a significant risk to the user. Second, they are often contaminated by direct exposure to aerosolized droplets during use and therefore contamination levels can be high. Finally, respirators are constructed of porous materials that cannot easily be cleaned or wiped. At this time, recommendations on UV dosage levels for respirators is >1000 mJ/cm2 to account for these factors.4, 6
Maximum decontamination/reuse cycles are currently between three and five. This is limited because UV light, and actual use, reduces the integrity of the elastic straps. UV dosages for decontamination of ambulance boxes, rooms, etc. surfaces, such as walls, cabinets, doors, etc. is lower at 50-100 mJ/cm2 depending on the contaminant.
A summary of common contaminants, with references, is given in the ClorDiSys UV Data Sheet Rev. 12-2020. This is because those are hard, non-porous surfaces and this is a secondary decontamination operation. In the following sections we will present our procedures and recommended dosage times which should be typical for the commercially available bulbs we have used.
N95 Decontamination Unit (the “Decontaminator”)
Build Information
The parts needed to construct the N95 Decontamination Unit are provided in Table 1. We have not provided direct links to suppliers because we have found availability of parts, especially the UVC bulbs and ballasts, to vary. Suppliers can be found online via internet search, or at local hardware stores, using the descriptions in Table 1. Note that there are several manufacturers of UVC bulbs and ballasts; the manufacturers listed are those we were able to source and not an endorsement of those manufacturers. Sample pictures of items are also shown in the figures for visual reference.
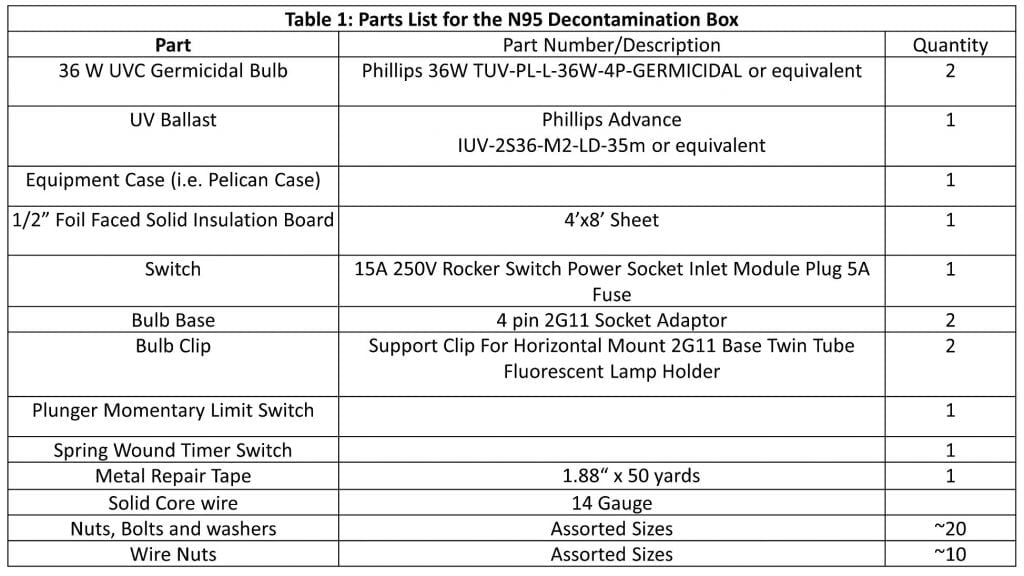
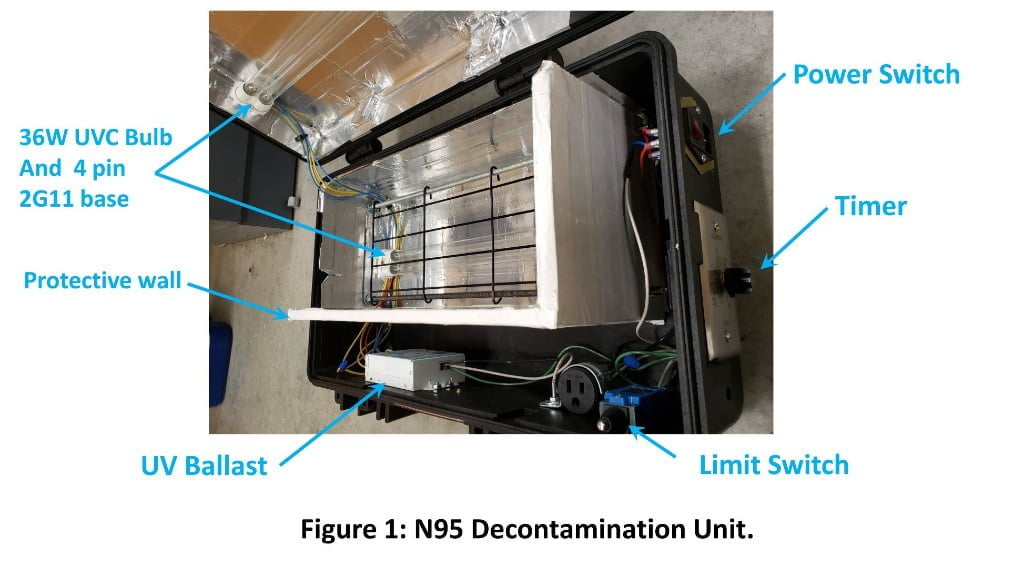
The system is housed in a large, thermoplastic equipment case. Our case measured 22”x14”x8” which long enough for the bulbs and mounts, and deep enough for two bulbs plus the N95 masks. We can fit three to four N95 masks without overlap in the case at a time. The power switch and spring wound timer were mounted through the outer wall of the case (Figure 1). We found that creating a cardboard template for the cut-outs and a Dremel with a cutting wheel work well to cut these out.
The ballast and bulb base were mounted inside the case via bolts through the case. A limit switch was installed to cut power to the bulb if the case is opened during use, which prevents UV exposure. The limit switch was mounted to the case at the case opening with a small steel angle bracket as a striker plate. Metal repair tape was used to line the case providing reflective surfaces. Internal walls were cut from foam insulation board to isolate the electronics from the UV light during operation.
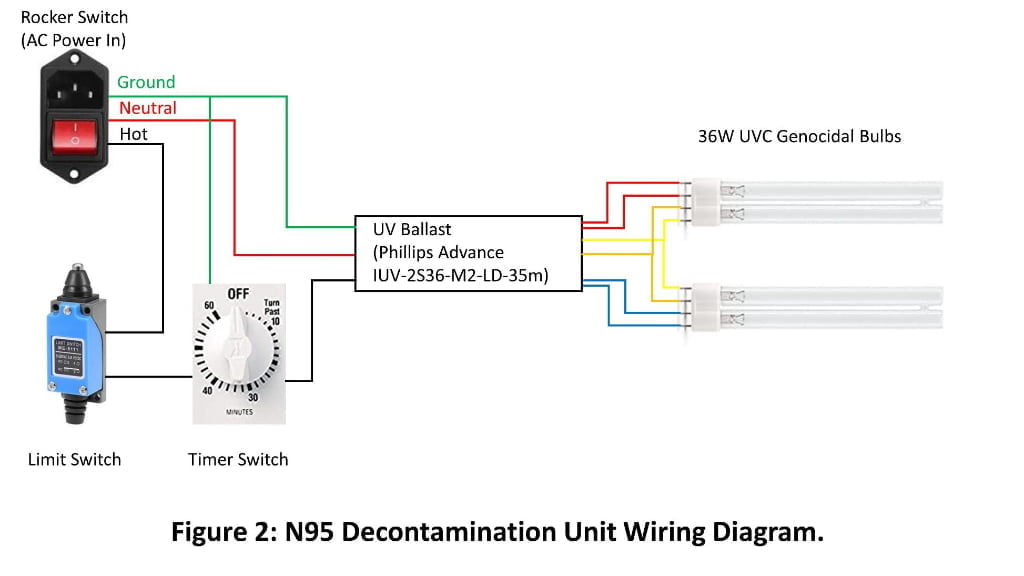
A wire rack was added to the treatment area to set the respirators on. We used colored 14-gage solid core wire when constructing the system. The wiring diagram for the two-bulb system is provided in Figure 2. Readers should refer to the ballast manufacturer’s wiring diagram to confirm connections. A single bulb system can be constructed and ballast wiring directions should follow manufacturer specifications.
Dosage and Performance
Bulb irradiance was measured using a self-built Arduino Uno light sensor system. This characterization was performed with the sensor approximately 3.5 cm away from the bulb on the grating where the bottom of a N95 respirator would sit. The irradiance was Ee= 3.5 mW/cm2 and the UV dosage, He=1000 J/cm2, was reached in approximately six minutes.
Procedure
Providers doff PPE per protocols. The N95 is placed in a paper lunch bag for storage and transportation to our station where the UV box resides. The provider removes the contaminated N95 from the bag using proper PPE and places it on the rack in the box with the outside of the mask facing the top bulb. Masks should not be overlapped to prevent shadows. The contaminated paper bag is disposed of. The box is closed and secured. A 10-minute dosage time is dialled into the mechanical timer and the device is turned on via a power switch. Once the cycle is completed the provider marks their respirator with a hash mark to provide a visual record of the number of cycles the mask has gone through.
The provider then tests the straps for integrity. The cycle is recorded on a log sheet with the date, provider name, number of cycles the mask has undergone, and a notation if the mask was returned to service. To date we have not noticed loss of strap integrity for the masks that have been taken out of service due to maximum number of cycles. Notes: 1: Masks are limited to 5 UVC cycles; 2: the mask should be warm after treatment and a smell ozone should be present when the lid is opened; 3: masks that have been grossly soiled with body substances are immediately discarded after use.
The UV box is multipurpose and can be used for secondary decontamination of other small reusable equipment. The most obvious of these is laryngoscopes and blades. For these objects, dosage recommendations are 100 mJ/cm2 and should be given after primary disinfection is performed. This treatment is not recommended for objects that could be broken down by UV exposure (e.g. stethoscopes) or intended to be used on reusable instruments (e.g. disposable plastic video laryngoscope blades).
UV Tower Unit (the “Roominator”)
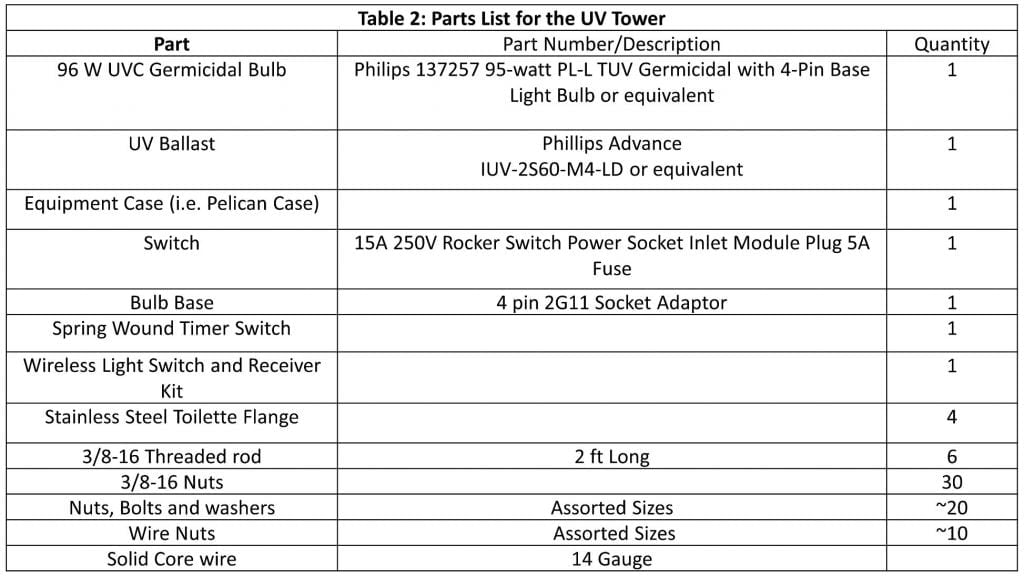
Build Information
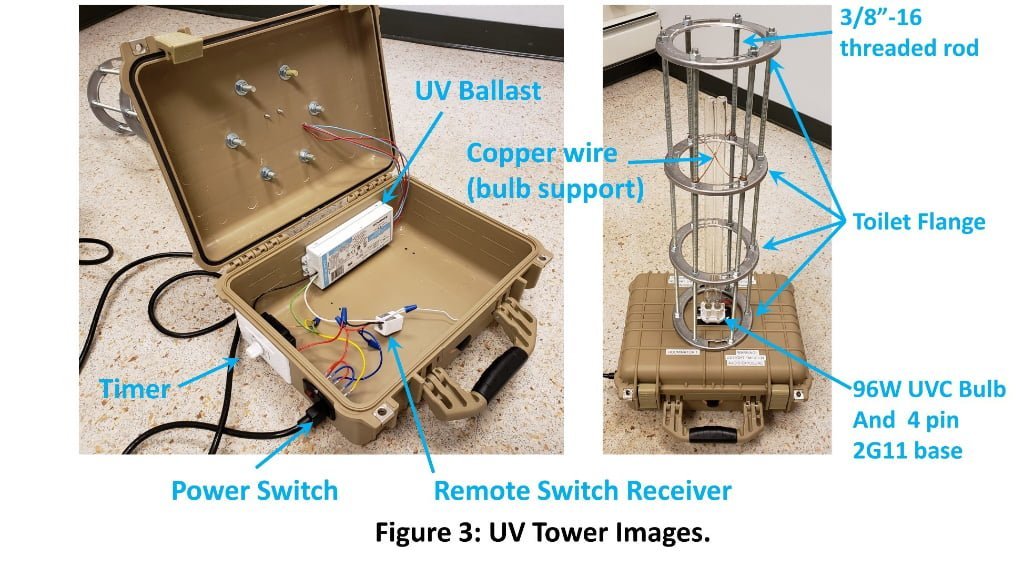
The construction of the UV Tower Unit is similar to the N95 unit with the following exceptions. Parts are listed in Table 2. A 95W UVC bulb, and appropriate ballast, were used to increase output due to the longer distances involved in room decontamination. The case had a smaller footprint (11 7/8” x 9” x 5 5/16”) as it was the base for the unit (Figure 3). The bulb base was mounted to the outside of the case in the middle of the top face.
The threaded rods and stainless steel toilet flanges were used to construct a protective cage around the bulb. The toilet flanges were a convenient and inexpensive part to give the cage form. The only modification that needed to be made to the flanges was expansion of the holes in the flange with a hand drill to accommodate the threaded rod. Steel was chosen as UV can breakdown plastics. Nuts were used above and below each flange to secure their locations.
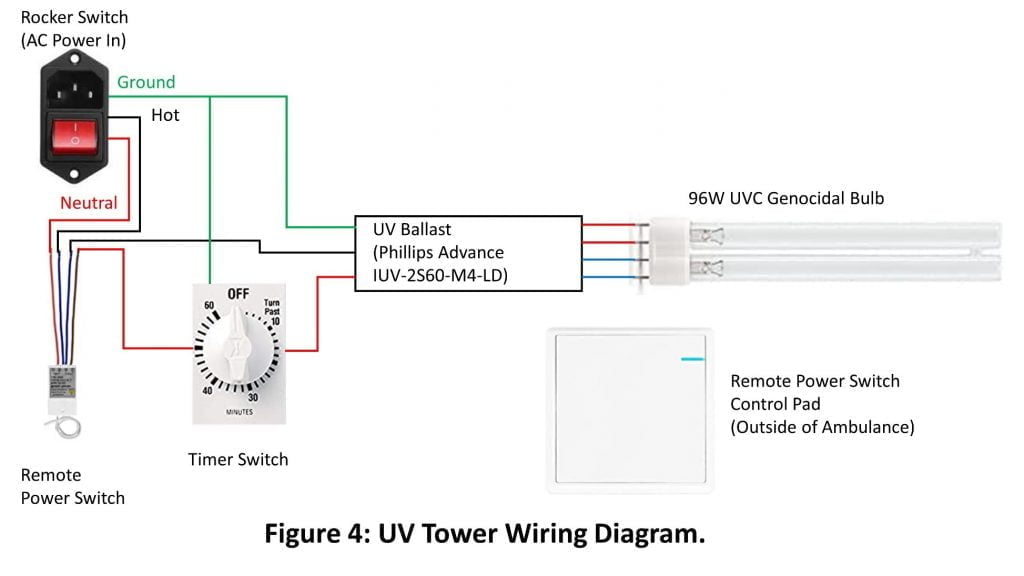
Bare 14 gage copper wire was used to prevent the vertically mounted bulb from moving by passing through the middle of the twin bulb tubes and winding to the threaded rod. A remote control switch was added to the wiring so that the tower unit could be placed inside of the ambulance box and activated remotely to prevent UV exposure for the user. The wiring diagram is provided in Figure 4.
Dosage and Performance
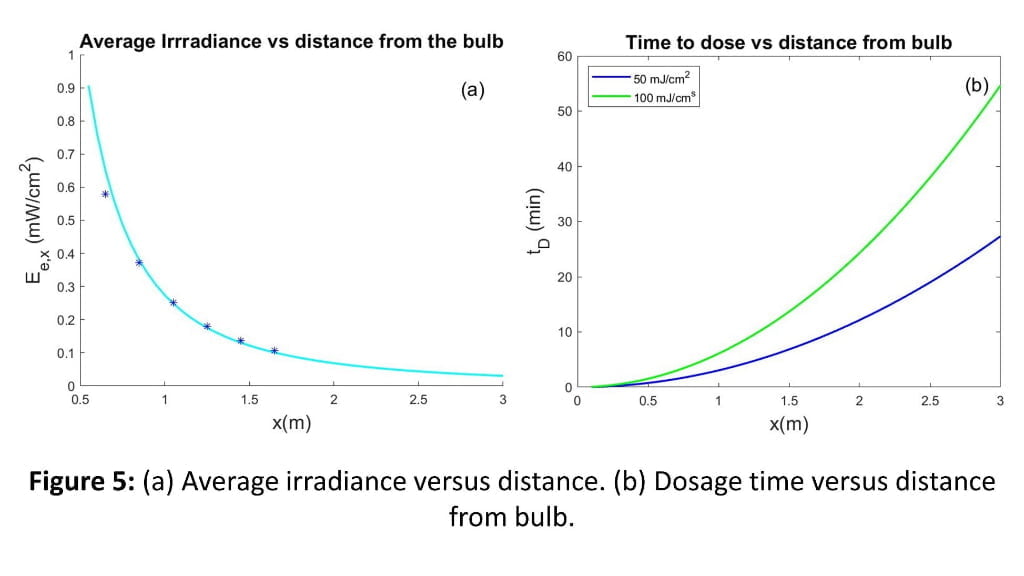
Measurements of the output from the UV tower unit were also performed using the Arduino Uno-based sensor system to determine irradiance as a function of distance from the bulb. The experiments were performed by placing the UV sensor at distances ranging from 0.65-1.65 m away from the bulb, (Figure 5a). Equation2 was used to provide predicted irradiance at any location (green line in Figure 5a) and showed good agreement with the measured data. Figure 5b shows the UV exposure time in minutes to reach those dosage levels versus distance from the bulb.
This figure served as a guide for setting dosage times based on the maximum distance in the box from the bulb. Our ambulance boxes have a maximum distance of approximately 2 m (6.5 ft) from the center to the outside of the box, which based on the data in Figure 5b corresponds to dosage times of approximately 22 minutes to reach He=100 mJ/cm2.
The measured values were verified in an ambulance box by placing UVC dosimeter cards (American Ultraviolet) at various locations in the ambulance box. These cards are light sensitive and change color based on He with color guides for 50 and 100 mJ/cm2. All locations were confirmed to reach He>100 mJ/cm2 level by 30 minutes. A UV dosage card was also placed on the outside of the rear window to investigate UV leakage through the windows and no change in color was detected for 60 minutes of exposure. This indicated that closed doors and windows were sufficient protection from outside UV exposure. Visible light emitted by the bulb does pass through the window which can be used to verify the bulb is on.
Procedure
The primary decontamination of ambulance box is performed per normal procedures using an FDA approved disinfectant, following the manufactures’ recommendations for use. The stretcher and cardiac monitor are removed and the UV tower is placed in the middle of the box on a wooden stand. The tower is plugged into an AC outlet in the box and the timer is set for 30 minutes.
This dose provides He>100 mJ/cm2 at all locations in our box and simplifies the protocol for providers. The doors to the box are closed and the UV tower is activated using a remote control switch. Once the cycle is finished, the box is opened and ventilated to disperse any built-up ozone. It is noted that the only significant region not exposed to UV light is directly be behind the captain’s chair due to its shadow.
The UV tower system can also be used in other settings where the room size is consistent with the bulb output (e.g. small exam rooms, lounges, etc.). The low cost of the system makes it ideal for settings where budgets prohibit the purchase of hospital specific UV tower systems.
We have constructed two of these systems that are currently in use at Clarkson University. The first system is being used in the campus health center exam rooms. The second system is being used by facilities staff who are currently responsible for cleaning dorm rooms that house quarantined students who have been exposed to COVID-19.
Conclusions
The COVID-19 pandemic has served as a reminder to the first responder community about the importance of personal protection and proper decontamination. This manuscript describes two UVC systems that can be used to decontaminate equipment in a prehospital setting. The systems are low cost using parts that can be found online or at local hardware stores and can be constructed easily and quickly with basic tools.
We have measured the light power output levels in these systems and based our protocols on those measured levels and published scientific recommendations.
For disposable N95 respirators, a level of greater than 1000 mJ/cm2 can be reached in six minutes, which we exceed with our 10-minute treatment. Respirators are limited to five decontamination cycles. In our ambulance boxes we reach >100 mJ/cm2 at all surfaces using our 30-minute treatment time. We recommend that any agency that builds and uses either of these systems verify their system outputs and confirm dosage times using dosimeter cards. This system has not received FDA clearance and users assume all risk associated with its use.
Acknowledgements
We would like to thank Brian Crabtree who also developed a similar N95 system and was a helpful sounding board as we designed our system.
References
- Viscusi DJ, Bergman MS, Eimer BC, Shaffer RE. Evaluation of Five Decontamination Methods for Filtering Facepiece Respirators. Ann Occup Hyg. 2009;53(8):815-27. doi: 10.1093/annhyg/mep070. PubMed PMID: WOS:000271813500006.
- Fisher EM, Shaffer RE. Considerations for Recommending Extended Use and Limited Reuse of Filtering Facepiece Respirators in Health Care Settings. J Occup Environ Hyg. 2014;11(8):D115-D28. doi: 10.1080/15459624.2014.902954. PubMed PMID: WOS:000337946700002.
- Lindsley WG, Martin SB, Thewlis RE, Sarkisian K, Nwoko JO, Mead KR, et al. Effects of Ultraviolet Germicidal Irradiation (UVGI) on N95 Respirator Filtration Performance and Structural Integrity. J Occup Environ Hyg. 2015;12(8):509-17. doi: 10.1080/15459624.2015.1018518. PubMed PMID: WOS:000357148900001.
- Mills D, Harnish DA, Lawrence C, Sandoval-Powers M, Heimbuch BK. Ultraviolet germicidal irradiation of influenza-contaminated N95 filtering facepiece respirators. Am J Infect Control. 2018;46(7):E49-E55. doi: 10.1016/j.ajic.2018.02.018. PubMed PMID: WOS:000436956200002.
- Fischer RJ, Morris DH, van Doremalen N, Sarchette S, Matson MJ, Bushmaker T, et al. Effectiveness of N95 Respirator Decontamination and Reuse against SARS-CoV-2 Virus. Emerg Infect Dis. 2020;26(9):2253-5. doi: 10.3201/eid2609.201524. PubMed PMID: WOS:000566799800047.
- US Centers for Disease Control and Prevention, Implementing Filtering Facepiece Respirator (FFR) Reuse, Including Reuse after Decontamination, When There Are Known Shortages of N95 Respirators [cited 2020 December 2, 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html.

Douglas Bohl, PhD (Mechanical Engineering), AEMT, is an Associate Professor in the Department of Mechanical and Aeronautical Engineering, faculty advisor for Clarkson University EMS and a volunteer AEMT with the Potsdam (NY) Volunteer Rescue Squad.

Christopher Towler, PT, DPT, GCS, CEEAA, AEMT-P, is an Assistant Clinical Professor in the Physical Therapy Department at Clarkson University and a volunteer NYS AEMT-P with the Potsdam (NY) Volunteer Rescue Squad.




